Pharmacy Residency Program
Welcome to the Jackson-Madison County General Hospital PGY1 Pharmacy Residency Program Website. PGY1 residency training is a challenging but rewarding experience. I commend you for your commitment to your education and the profession of pharmacy. Jackson-Madison County General Hospital (JMCGH) is a large tertiary care community hospital in rural West Tennessee, and the flagship institution of West Tennessee Healthcare. Our service area includes West Tennessee, parts of the Missouri bootheel, and northern Mississippi. This large service area gives our institution the depth and breadth of patient experiences typically seen in a large academic medical center but nestled in a mid-size town with a welcoming atmosphere. The Department of Pharmacy is integral across all of West Tennessee Healthcare. We have relationships with two area colleges of pharmacy, and conduct both introductory and advanced practice experiences at our institution.
Specifically, the Jackson-Madison County General Hospital PGY1 pharmacy residency prepares pharmacists for community-based hospital practice, to serve as experiential adjunct faculty for a college of pharmacy, and/or to pursue second-year post-graduate residency training in a focused area of practice.
Thank you for your interest in our PGY-1 residency program.
Sincerely,
Dylan Wilson, Pharm.D., BCPS, AACC
PGY-1 Residency Program Director
Jackson-Madison County General Hospital Purpose
The purpose of the Jackson-Madison County General Hospital PGY-1 pharmacy residency is to prepare pharmacists for community-based hospital pharmacy practice, to serve as experiential adjunct faculty for a college of pharmacy, and / or to pursue second year post-graduate residency training in a focused area of practice.
Program Information/Application
Hospital Information
- 642-bed tertiary care center
- Non-profit institution
- Serves 19 West Tennessee counties: over 500,000 persons
- Flagship hospital of West Tennessee Healthcare
- Contains 6 Intensive Care Units (MICU, SICU, CCU, CVICU, NeoICU, NeuroICU) providing 120 ICU beds
- Emergency Department treats ~100,000 patients per year
- Average daily census is 450
- Employees 76 licensed pharmacists
Program Details
- ASHP Accredited
- Number of Residents: 4
- Duration of Program: 12 months
- Stipend: $49,000
- Benefits
- Paid Earned Time: 10 days per year
- Sick Time: 6 days per year
- Administrative Leave: granted for professional activities
- Interview Leave: up to 3 days with documentation of interview
- Health Insurance
- WTH Benefits Page
Application Requirements/Qualifications
- Interview required
- PharmD or equivalent experience
- Eligibility for licensure in Tennessee with expected licensed by date of September 30.
- U.S. citizenship required
- Application must be submitted through PhORCAS
- PhORCAS Requirements
- General Application
- Letter of Intent
- Curriculum vitae
- Official copy of college/university transcript (Pharmacy School only)
- Three letters of recommendations using the ASHP Standardized Residency Application Recommendation Request Form
- Application deadline: January 2, 2024
ASHP Program Code: 54007
NMS Code: 183913
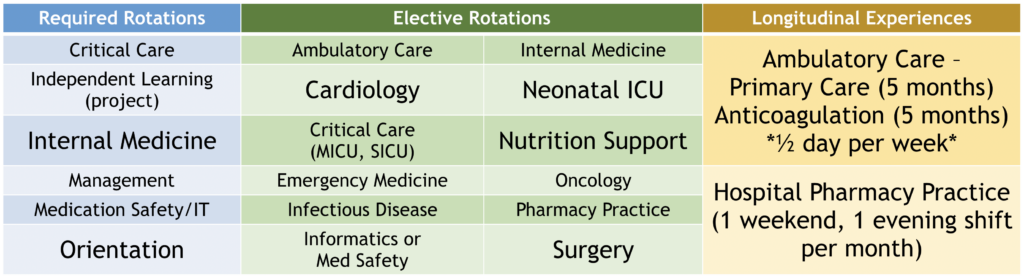
Residency Rotation Opportunities
Projects and Presentations
- Residency project for presentation at the MidSouth Pharmacy Residency Conference
- Prepare and present one Medication Use Evaluation (MUE)
- Attend P&T Committee Meetings
- Attend and take minutes for an assigned hospital committee throughout the year
- Prepare a Drug Monograph and Therapeutic Review for presentation to P&T Committee
- Prepare a PharmaGram
- Prepare and present a Continuing Education (CE) presentation to the West Tennessee Pharmacists Association
- Obtaining Teaching and Learning Certificate*
- Lecture opportunities with Union University College of
Pharmacy/University of Tennessee Family Medicine Residents*
*=optional
Current Residents

Han Na Cho, PharmD
Hometown: Murfreesboro, Tennessee
Undergraduate Education: University of Tennessee at Knoxville
Pharmacy School Education: University of Tennessee College of Pharmacy
Why I chose JMCGH PGY-1 Residency Program: I chose JMCGH because of the vast opportunities that this program has to offer. The JMCGH family is so welcoming and provides a positive learning environment for residents. The philosophy of putting the patient first aligns with my goals to provide the best quality health care. I know JMCGH residency program will provide me many opportunities to grow as a well-rounded pharmacist.

Sydney Duffy, PharmD
Hometown: Middleton, Tennessee
Undergraduate Education: Baptist Health Sciences University
Pharmacy School Education: Union University College of Pharmacy
Why I chose JMCGH PGY-1 Residency Program: Through working at JMCGH during school, I was able to get an in-depth look at the pharmacy department and residency program. The pharmacy team at JMCGH is the selling point that sets this program apart from others. The pharmacists are passionate about the profession and providing the best patient care possible. I believe JMCGH’s program will help me expand on my pharmacy knowledge and experience. Additionally, I feel this program provides diverse patient-care settings that will afford me opportunities to practice specialized pharmacy.

Melissa Rinks, PharmD
Hometown: Eads, Tennessee
Undergraduate Education: University of Tennessee at Knoxville
Pharmacy School Education: University of Tennessee College of Pharmacy
Why I chose JMCGH PGY-1 Residency Program: I chose JMCGH not only because of the variety of patient care specialties offered, but also because of the wonderful culture of West Tennessee Healthcare. Everyone is extremely welcoming, encouraging, and dedicated to their patients. I wanted a program to strengthen my clinical confidence while also providing a supportive environment to help me grow as a new pharmacist. I can say without a doubt that this program provides just that, in addition to some smiles along the way!

Alexandria “Ali” Thompson, PharmD
Hometown: Scotts Hill, Tennessee
Undergraduate Education: Union University
Pharmacy School Education: Union University College of Pharmacy
Why I chose JMCGH PGY-1 Residency Program:
I chose JMCGH because of my wonderful experience here as a student. My preceptors were genuine and supportive, all while pushing me to perform at my best. The JMCGH residency program offers a variety of learning environments and opportunities that will aid me in achieving my career goals!
Meet the Preceptors

Sherry Osborne, RPh
Hometown: Medina, Tennessee
Undergraduate Education: Jackson State Community College
Pharmacy School Education: University of Tennessee College of Pharmacy
Practice Interests: Administration
Hobbies: My dogs!!
What I love most about practicing at JMCGH: I love the employees and just knowing that what we do each day is helping somebody to go home!!
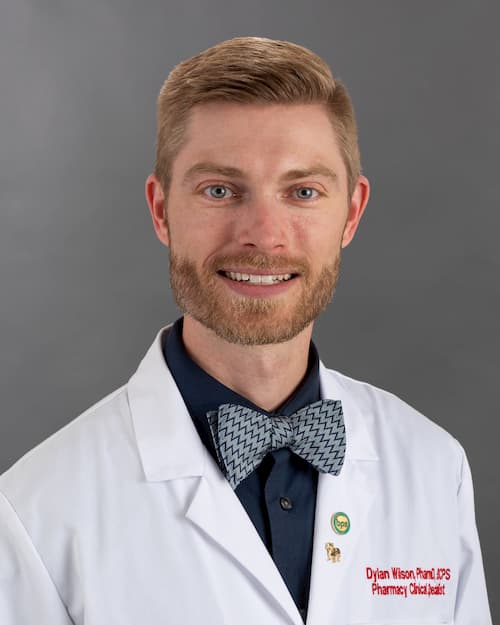
Dylan Wilson, PharmD, BCPS
Hometown: Flint, MI
Undergraduate Education: Ferris State University
Pharmacy School Education: Ferris State University
Residency: PGY-1 St. Joseph Mercy Hospital in Ann Arbor, MI
Practice/Research Interests: Cardiology specifically cardiovascular surgery and PCI and Research projects
Hobbies: Coaching my kids’ teams, woodworking, and running
What I love most about practicing at JMCGH: I love the people. People make the difference in all of the areas that I’m involved with from the pharmacy department to the CVICU.

Ashley Bynum, PharmD, BCPS, BCCCP
Hometown: Kennett, MO
Undergraduate Education: University of Mississippi
Pharmacy School Education: University of Mississippi School of Pharmacy
Residency: PGY-1 North Mississippi Medical Center in Tupelo, MS
Practice/Research Interests: Critical Care
Hobbies: playing piano, reading, spending time outdoors with my 3 dogs, and family movie nights
What I love most about practicing at JMCGH: I love the sense of community not just within the pharmacy department but within the whole hospital. I feel like part of a team providing the best care possible to patients in the ICU. I look forward to coming to work each morning which means a lot to me.
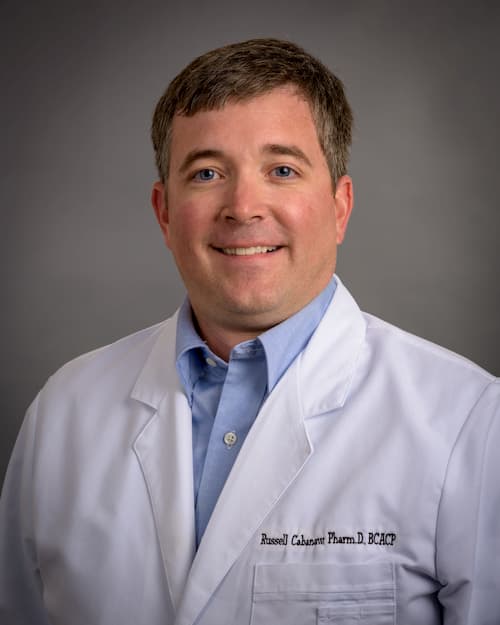
Rusty Cabanaw, PharmD, BCACP
Hometown: Jackson, Tennessee
Undergraduate Education: Union University
Pharmacy School Education: University of Tennessee College of Pharmacy
Residency: PGY-1 University of Tennessee College of Pharmacy/Holston Medical Group
Practice Interests: Ambulatory Care
Hobbies: Running, reading, and UT Football/most sporting events
What I love most about practicing at JMCGH: I enjoy the opportunity to practice in my hometown, to establish patient relationships, and to work with other healthcare providers in helping to improve patient’s healthcare.

Austin Camp, PharmD, BCPS
Hometown: Jackson, TN
Undergraduate Education: Union University
Pharmacy School Education: Union University College of Pharmacy
Residency: PGY-1 Baptist Memphis Hospital in Memphis, TN
Practice/Research Interests: Critical Care, Toxicology, and Infectious Disease
Hobbies: Music, Movies, and Memphis Grizzlies
What I love most about practicing at JMCGH: I love the opportunity to work with a multidisciplinary team in the SICU.

Sonia Carter, PharmD, BCPS
Hometown: Jackson, TN
Undergraduate Education: Harvard University
Pharmacy School Education: Union University College of Pharmacy
Residency: PGY-1 Jackson-Madison County General Hospital in Jackson, TN
Practice/Research Interests: Internal Medicine and Antimicrobial Stewardship
Hobbies: Spending quality time with family and friends, dog mom, and reading
What I love most about practicing at JMCGH: I love the wonderful work atmosphere with a skilled pharmacy team.

Greg Gibson, PharmD
Hometown: Meridian, MS
Undergraduate Education: Mississippi State University
Pharmacy School Education: Bachelor of Pharmacy from University of Mississippi, Doctor of Pharmacy from University of North Carolina
Practice/Research Interests: Neonatal and Pediatric Medicine
Hobbies: Cooking, gardening, spending time with family as I’m the father of twins that are in the second year of college.
What I love most about practicing at JMCGH: I enjoy the friendly working environment of JMCGH. The people I work with in the pharmacy and in the pediatric and neonatal areas make it fun to come to work each day. I know we have a voice in patient care and other healthcare professionals value our opinion.

Courtney Guinn, PharmD
Hometown: McLemoresville, TN
Undergraduate Education: University of Tennessee at Martin
Pharmacy School Education: Union University College of Pharmacy
Residency: PGY-1 Jackson-Madison County General Hospital in Jackson, TN
Practice Research/Interests: Emergency Medicine, Critical Care, and Cardiology
Hobbies: Spending time with family, vacationing to the beach, reading, and hunting
What I love most about practicing at JMCGH: I love the community-based atmosphere and the autonomy to develop additional pharmacy services. I love the receptiveness of providers and nurses. We are all like one big family supporting each other to provide the best care for our patients!

Zachery Halford, PharmD, BCOP, BCPPS
Hometown: Salt Lake City, UT
Undergraduate Education: University of Utah
Pharmacy School Education: University of Utah
Residency: PGY-1 Tripler Army Medical Center in Honolulu, HI
Practice/Research Interests: Pediatrics, Hematology/Oncology
Hobbies: Fitness, golfing, and making sure my kids survive gymnastics
What I love most about practicing at JMCGH: JMCGH is a large, progressive hospital with a variety of subspecialties, but it feels like a community hospital.
Jordan Harrington, PharmD
Hometown: Bath Springs, TN
Undergraduate Education: University of Tennessee at Martin
Pharmacy School Education: University of Tennessee College of Pharmacy
Residency: PGY-1 Jackson-Madison General Hospital in Jackson, TN
Practice/Research Interests: Infectious Disease, Nutrition, and Pediatrics
Hobbies: Running, cycling, traveling, and cooking
What I love most about practicing at JMCGH: I love that working at JMCGH feels like being part of one large community, both within the pharmacy department and other departments throughout the hospital.
Jeremy Hicks, PharmD, BCPS
Hometown: Ooltewah, TN
Undergraduate Education: University of Tennessee at Chattanooga
Pharmacy School Education: University of Tennessee College of Pharmacy
Residency: PGY-1 Veterans Affairs Medical Center in Memphis, TN
Practice/Research Interests: Internal medicine/Nutrition Support
Hobbies: I grew up doing projects around the house with my dad. So, naturally I became “Mr. Fix It” like him. If you have the right tools you can do just about anything. I like anything that flies…real planes, model planes, home-made rockets. At night I look at the stars, planets, constellations, and the international space station while walking with my wife or taking the dog out. I’m amazed by God’s creation.
What I love most about practicing at JMCGH: The pharmacy is an extension of my own family, and we work well together. An added benefit is getting to work with some intelligent, talented people. It is also important that pharmacy is respected by our administration, doctors, NPs, PAs, nurses, and others at JMCGH.

Jamie Hopkins, PharmD, BCIDP
Hometown: Manchester, TN
Undergraduate Education: Mercer University
Pharmacy School Education: University of Tennessee College of Pharmacy
Residency: Veteran Affairs Medical Center in Memphis, TN
Practice/Research Interests: Antimicrobial Stewardship
Hobbies: Reading, running, and spending time outdoors with my husband and kids
What I love most about practicing at JMCGH: What attracted me to JMCGH almost 20 years ago was the opportunity to help create something new. The people I work with keep me here now. The pharmacists, technicians, residents, and students work hard to take care of the people here. We work well together and have a good time while doing so.

Bethannee Horn, PharmD, BCPS
Hometown: Monticello, Arkansas
Undergraduate Education: University of Arkansas
Pharmacy School Education: Union University College of Pharmacy
Residency: PGY-1 Jackson-Madison County General Hospital in Jackson, Tennessee
Practice Interests: Internal Medicine
Hobbies: Traveling, reading, and spending time with family, friends, and my dogs
What I love most about practicing at JMCGH: I love the relationships I have built with both my pharmacy team and other healthcare professionals. I also appreciate the daily opportunities I have to help patients.

April Ingason, PharmD
Hometown: Bartlett, TN
Undergraduate Education: University of Memphis
Pharmacy School Education: Union University College of Pharmacy
Residency: PGY-1 Jackson-Madison County General Hospital in Jackson, TN
Practice Interests: Perioperative
Hobbies: Family time, cooking, traveling, and yoga
What I love most about practicing at JMCGH: I love being able to develop the role of a surgery pharmacist by expanding clinical services offered in the surgery department. Working in surgery is like belonging to a community; we are all here to work together to take care of our patients. I enjoy the overall inviting atmosphere of the hospital; Jackson General is an amazing place to work!

Kristen Lee, PharmD, BCIDP
Hometown: Jackson, TN
Undergraduate Education: University of Mississippi
Pharmacy School Education: University of Mississippi School of Pharmacy
Practice/Research Interests: Antimicrobial Stewardship
Hobbies: Raising 5 children and watching them play any and all sports
What I love most about practicing at JMCGH: I love the camaraderie among all the pharmacists I work with at JMCGH the most. The pharmacists here genuinely care about each other, as well as our students and residents. In addition, we strive to take exemplary care of our patients.

Taylor Mathis, PharmD, MS, BCACP
Hometown: Madison, MS
Undergraduate Education: University of Mississippi
Pharmacy School Education: University of Mississippi School of Pharmacy
Residency: 2-Year Community Pharmacy Administration Residency with Kroger Health and the University of Cincinnati James L. Winkle College of Pharmacy
Practice/Research Interests: Chronic Disease Management and Women’s Health
Hobbies: Quality time with family, crossword puzzles, and coloring books
What I love most about practicing at JMCGH: I love having the opportunity to work with physicians and nurses to develop high-quality, individualized care plans for patients.

Andrew Martin, PharmD
Hometown: Rives Junction, MI
Undergraduate Education: Ferris State University
Pharmacy School Education: Ferris State University College of Pharmacy
Residency: PGY-1 University of Utah Hospitals and Clinics
Practice/Research Interests: Medication safety and quality, drug information, and informatics
Hobbies: Parenting and beekeeping
What I love most about practicing at JMCGH: JMCGH offers a place to work and grow with people who care and are continually working to advance the practice of pharmacy.

Bethany McMackin, PharmD, BCPS
Hometown: Collierville, TN
Undergraduate Education: University of Arkansas
Pharmacy School Education: University of Tennessee College of Pharmacy
Residency: PGY-1 Jackson-Madison County General Hospital in Jackson, TN
Practice/Research Interests: Emergency Medicine
Hobbies: Sports, music, traveling, and reading
What I love most about practicing at JMCGH: I love the atmosphere of JMCGH. There is an open dialogue present between pharmacy and other healthcare professionals that creates a working environment of mutual respect.

Ashley Pugh, PharmD, BCACP
Hometown: Henderson, Tennessee
Undergraduate Education: Union University
Pharmacy School Education: Union University College of Pharmacy
Residency: PGY-1 Union University College of Pharmacy/Kroger Pharmacy
Practice/Research Interests: Chronic disease management, especially diabetes, hypertension, hyperlipidemia, asthma, and COPD; immunizations; medication access; teaching and learning
Hobbies: Traveling, running/working out, waterskiing, and reading
What I love most about practicing at JMCGH: I love the opportunity to both practice and teach students and residents as part of an interprofessional team.
Brian Shaw, PharmD, BCPS
Hometown: Martin, TN
Undergraduate Education: University of Tennessee at Martin
Pharmacy School Education: University of Tennessee College of Pharmacy
Practice Interests: Internal Medicine
Hobbies: Fishing and golf
What I love most about practicing at JMCGH: I have worked for JMCGH for over 13 years, and I can say that almost no two days are the same. I like being able to see and learn new things, and that is easy to do here due to the variety of experiences at JMCGH. What I like most is helping take care of patients. Helping patients with their medicines gives me a fulfilled purpose in the work I do each day.

Jessica Smith, PharmD, BCPS
Hometown: Jackson, TN
Undergraduate Education: Jackson State Community College and Union University
Pharmacy School Education: University of Tennessee College of Pharmacy
Residency: PGY-1 Jackson-Madison County General Hospital in Jackson, TN
Practice/Research Interests: Cardiac Step-down, Pain management, and Congestive Heart Failure
Hobbies: Baking and growing herbs
What I love most about practicing at JMCGH: I enjoy getting to work with students and residents because it thrills me to watch them grow in knowledge and confidence as they progress.

Alydia Snyder, PharmD, BCNSP
Hometown: West Helena, AR
Undergraduate Education: Union University
Pharmacy School Education: Union University College of Pharmacy
Residency: PGY-1 Jackson-Madison County General Hospital in Jackson, TN
Practice/Research Interests: Nutrition Support and Antimicrobial Stewardship
Hobbies: Spending time with my husband and 3 kids, reading, and going to the beach
What I love most about practicing at JMCGH: I love the people I work with and the family atmosphere we have!

Brad Spencer, PharmD, BCCCP
Hometown: Collierville, TN
Undergraduate Education: Union University
Pharmacy School Education: Union University College of Pharmacy
Residency: PGY-1 Jackson-Madison County General Hospital in Jackson, TN
Practice/Research Interests: Small group teaching, drug allergy, social media influence on public’s science/medicine perceptions
Hobbies: Playing with my children, biking, and coaching soccer
What I love most about practicing at JMCGH: I love the wide variety of services and patient conditions.

JoLeigh Sutton, PharmD, BCPS
Hometown: Chattanooga, TN
Undergraduate Education: Carson-Newman University
Pharmacy School Education: Samford McWhorter School of Pharmacy
Residency: PGY-1 UAB Hospital in Birmingham, AL
Practice/Research Interests: Informatics and Internal Medicine
Hobbies: I am a singer, wife, and mother to three beautiful children. I also dabble in painting, crafting, and cake making.
What I love most about practicing at JMCGH: I love that I can make an impact on patient care on a daily basis either directly or indirectly. I am also blessed to work with a staff that is compassionate, friendly, and treats each other like family. We can do hard things together!

Jodi Taylor, PharmD, BCPS, BCCCP
Hometown: Trenton, TN
Undergraduate Education: Middle Tennessee State University
Pharmacy School Education: University of Tennessee College of Pharmacy
Residency: PGY-1 Veterans Affairs Medical Center in Memphis, TN
Practice/Research Interests: Critical Care and Cardiology
Hobbies: Gardening
What I love most about practicing at JMCGH: JMCGH is a perfect blend of community and academic practice with a hometown/family feel!
Christy Waggoner, PharmD, BCPS
Hometown: Jackson, TN
Undergraduate Education: University of Tennessee at Knoxville
Pharmacy School Education: University of Tennessee College of Pharmacy
Residency: PGY-1 Jackson-Madison County General Hospital in Jackson, TN
Practice Interests: Ambulatory Care
Hobbies: Traveling, reading, and playing with my two daughters
What I love most about practicing at JMCGH: I love building relationships with my patients the most.
Lyn Wells, PharmD
Hometown: Memphis, TN
Undergraduate Education: University of the South Sewanee, TN
Pharmacy School Education: University of Tennessee College of Pharmacy
Practice Interests: Oncology
Hobbies: Knitting, reading, listening to music, my dogs, and hunting/fishing
What I love most about practicing at JMCGH: I love the sense of family within the Department of Pharmacy along with the camaraderie felt within the Kirkland Cancer center as we all focus on the patients’ well being.
Former Residents
Resident Name | Year of Residency | Current Position | Practice Location |
Kaleb Adams | 2022-2023 | Clinical Pharmacist | Vital Care of Northwest Alabama – Florence, AL |
Minh Dong | 2022-2023 | Clinical Pharmacist | Jackson-Madison County General Hospital – Jackson, TN |
Nathan Heitz | 2022-2023 | Oncology Clinical Pharmacist | Jackson-Madison County General Hospital – Jackson, TN |
Jessie Roberts | 2022-2023 | Internal Medicine Clinical Pharmacist | Renown Health – Reno, NV |
Leanna Estredge | 2021-2022 | Clinical Pharmacist | Jackson-Madison County General Hospital – Jackson, TN |
Brittany Kelley | 2021-2022 | Clinical Pharmacist | Jackson-Madison County General Hospital – Jackson, TN |
Elliot Lea | 2021-2022 | Clinical Pharmacist | Wellmed Medical Management, Inc with Optum Care Delivery |
Kelsey Rowland | 2021-2022 | Clinical Pharmacist | Jackson-Madison County General Hospital – Jackson, TN |
Julianna Bolton | 2020-2021 | Clinical Pharmacist | Jackson-Madison County General Hospital – Jackson, TN |
Vanessa Gresham | 2020-2021 | Clinical Pharmacist | Huntsville Hospital – Huntsville, AL |
Fabrice Kamgang | 2020-2021 | Ambulatory Care Clinical Pharmacist | Christ Community Health Services – Jackson, TN |
Prestley Miller | 2020-2021 | Clinical Pharmacist | Jackson-Madison County General Hospital – Jackson, TN |
Sophie Dunavant | 2019-2020 | Ambulatory Care Clinical Pharmacist | Spartanburg Regional Healthcare System – Spartanburg, SC |
Bethannee Horn | 2019-2020 | Clinical Pharmacist | Jackson-Madison County General Hospital – Jackson, TN |
Hannah Smith | 2019-2020 | Ambulatory Care Clinical Pharmacist | Regional One Health – Memphis, TN |
Aaron Zuller | 2019-2020 | Clinical Pharmacist | Jackson-Madison County General Hospital – Jackson, TN |
Bethany McMackin | 2018-2019 | Emergency Medicine Clinical Pharmacist | Jackson-Madison County General Hospital – Jackson, TN |
Tyler Byrd | 2018-2019 | Community Pharmacist | C&C – Dyersburg, TN and Greene Pharmacy – Steele, MO |
Kathryn Jones | 2018-2019 | Internal Medicine Clinical Pharmacist | Ascension St. Vincent – Indianapolis, IN |
Hallie Smith | 2018-2019 | Clinical Pharmacist | Huntsville Hospital – Huntsville, AL |
Pamela Sanford | 2017-2018 | Oncology Clinical Pharmacist | Mayo Clinic – Rochester, MN |
Jordan Harrington | 2017-2018 | Clinical Pharmacist | Jackson-Madison County General Hospital – Jackson, TN |
Justin Emmons | 2017-2018 | Clinical Pharmacist | Baptist Health Hospital – Paducah, KY |
Sonia Carter | 2016-2017 | Internal Medicine Clinical Pharmacist | Jackson-Madison County General Hospital – Jackson, TN |
Sarah Ayers | 2016-2017 | Clinical Pharmacist | Jackson-Madison County General Hospital – Jackson, TN |
Emily Grissom | 2016-2017 | Clinical Pharmacist | Jackson-Madison County General Hospital – Jackson, TN |
April Ingason | 2015-2016 | Surgery Clinical Pharmacist | Jackson-Madison County General Hospital – Jackson, TN |
Courtney Guinn | 2015-2016 | Emergency Medicine Clinical Pharmacist | Jackson-Madison County General Hospital – Jackson, TN |
Anwesa Chakrabarti | 2015-2016 | Ambulatory Care Clinical Pharmacist | Vanderbilt University Hospital – Nashville, TN |
Alexis Luckey | 2014-2015 | Clinical Pharmacist | Advanced Therapeutic Applications, LLC |
Steven Maher | 2014-2015 | Clinical Pharmacist | Mercy Hospital at Jefferson – Festus, MO |
Nhung Dang | 2014-2015 | Clinical Pharmacist | OSF Healthcare – Peoria, IL |
Brad Spencer | 2013-2014 | Informatics Clinical Pharmacist | Jackson-Madison County General Hospital – Jackson, TN |
Matthew Bibb | 2013-2014 | Clinical Pharmacist | Ascension Saint Thomas Hospital – Nashville, TN |
Lacie Bradford | 2013-2014 | Clinical Pharmacist | Erlanger Health System – Chattanooga, TN |
Alydia Snyder | 2012-2013 | Clinical Pharmacist | Jackson-Madison County General Hospital – Jackson, TN |
Connie Sharkey | 2012-2013 | Pharmacist Manager and Research Analyst | The Knowledge Center at HCA – Nashville, TN |
Allyson Wunderlich | 2012-2013 | Clinical Pharmacist | Saint Thomas Rutherford – Murfreesboro, TN |
Christy Waggoner | 2011-2012 | Ambulatory Care Clinical Pharmacist | Jackson-Madison County General Hospital – Jackson, TN |
Hope Welch | 2011-2012 | Clinical Pharmacist | Baptist Memorial Hospital Golden Triangle – Columbus, MS |
Jessica Smith | 2010-2011 | Clinical Pharmacist | Jackson-Madison County General Hospital – Jackson, TN |
Liz Underwood | 2010-2011 | Clinical Pharmacist | AR Care – Searcy, AR |


